Silence = death: how stigma around HIV and AIDS persists
Have we learned from the failings of our history? Tessa analyses the roots of stigma and injustice towards individuals with HIV and AIDS, and recalls the social and medical evolution in HIV care leading up to the present day.
Content warning: this article contains mentions of homophobia and discrimination
COVID-19 was not the first viral epidemic with great societal implications. Starting in the late 1970s, the emergence of human immunodeficiency virus (HIV) had lasting consequences for the treatment of the LGBTQIA+ community. HIV is a virus that, if left untreated, can lead to acquired immune deficiency syndrome (AIDS). The virus can disrupt the activation of the immune response, making the infected person vulnerable to all kinds of pathogens that wouldn’t normally cause problems in a healthy person. HIV progresses into AIDS when there are almost no immune cells left, leading to severe health complications. When the HIV pandemic broke out in the 1980s, the primary group affected were gay, bi, and men who have sex with men (MSM). Although the LGBTQIA+ rights movement was gathering momentum at the time, sexualities other than heterosexuality were still widely not accepted. As a result, the virus became surrounded by negative associations and discrimination against the LGBTQIA+ community, and in particular, against men who have sex with men.
“The stigma and shame around the virus and the LGBTQIA+ community in the 1980s are not just historical issues, they still have a big impact today”
The stigma and shame around the virus and the LGBTQIA+ community in the 1980s are not just historical issues, they still have a big impact today. Bruno (41) is a physiotherapist working in London who, after receiving a HIV diagnosis, suffered from a continued silence surrounding HIV and AIDS. Ever since, Bruno has been devoted to “starting conversations about HIV, trying to break those stigmas'' that continue to surround the virus. These conversations remain both valuable and crucial today in work to end the epidemic.
HIV has been around for decades but research into understanding and treating the infection has taken time to develop due to taboos that surrounded the infection during the early phases of the 1980s epidemic. In 1981, several otherwise healthy gay men in the United States (US) reported symptoms of a failing immune system. They presented with rare conditions such as Pneumocystis carinii pneumonia (PCP), a lung infection, and Kaposi’s Sarcoma, an aggressive cancer. The underlying cause of these illnesses, and subsequent deaths, was unknown at the time. As only gay, bisexual, and other MSM seemed to be infected, the disease became colloquially known as ‘gay cancer’ and ‘gay-related immunodeficiency’ (GRID). People started blaming the gay community and criticising stereotypical understandings of the community’s lifestyle and ethos, using the virus as means to continue to discriminate against them. As a result of these harmful social narratives, people were not only afraid of the disease, but of the people who they incorrectly thought were the cause.
The term AIDS was first introduced by the Centres for Disease Control (CDC) in 1982, as part of the first case definition:
“A disease at least moderately predictive of a defect in cell-mediated immunity, occurring in a person with no known cause for diminished resistance to that disease”.
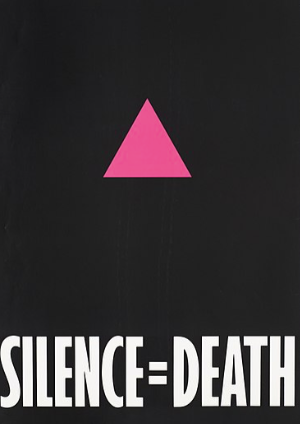
Image credit: ACT UP
This definition demonstrates large gaps in knowledge of the infection at the time, but funding for research remained minimal. As the disease had falsely become known as a ‘gay-related disease’, governmental bodies refused to acknowledge its emerging presence. In the US homosexuality was considered a mental illness and in the United Kingdom (UK) promotion of homosexuality was prohibited. Sexual orientations other than heterosexuality were (and sometimes still) not accepted. As a consequence, men who suspected having contracted HIV would refuse to get tested for fear of repercussions. Discrimination against the LGBQTIA+ community intensified during the AIDS epidemic, with detrimental consequences for both the progression of HIV and AIDS research and LGBTQIA+ rights.
It wasn’t until 1983 that the causative agent was discovered. The virologist Françoise Barré-Sinoussi and her team managed to isolate and identify the virus from a patient showing early symptoms of AIDS. Subsequent research began to focus on how the virus damages the body, but there was relatively little investigation into how it might spread from person to person. In the same year the virus was discovered, research suggested that the infection was transmitted through contact with bodily fluids such as blood and semen, and not through “casual contact” such as touch.
In the early 1980s, activism in the form of “visibility and public displays of resistance” was desperately needed, not only to obtain financial funding into research, but to remove the public’s negative associations with HIV and AIDS. The media continued to blame and discriminate against the LGBTQIA+ community*, whilst governments refused to speak about the subject. Headlines using phrases such as “the gay plague” and “doomed sons” maintained the public’s ignorance and fear towards the disease. The prime minister of the UK at the time, Margaret Thatcher, refused to support AIDS awareness campaigns, and US president Ronald Reagan remained completely silent about AIDS until an interview in 1985. The lack of concern, and perhaps the inability to see the severity of the situation from governments, led to research delays and allowed homophobic narratives to proliferate.
Opposing the AIDS-phobia were numerous groups of LGBTQIA+ groups and AIDS activists, such as Gay Men’s Health Crisis (GMHC) and the AIDS Coalition To Unleash Power (ACT UP). Started in 1981, GMHC aimed to raise money for research that was so desperately needed. In the years to follow, GMHC would publish safe sex guidelines, hold fundraisers, and set up multiple awareness campaigns—arguably making a bigger impact on the lives of HIV and AIDS patients than the US government. The famous “silence=death” poster created in 1986 by ACT UP activists was used to urge the governments to take action; by remaining silent more and more people would die.
“People started blaming the gay community and criticising stereotypical understandings of the community’s lifestyle and ethos, using the virus as means to continue to discriminate against them.”
Prejudices and misinformation surrounding HIV and AIDS were also countered by acts of solidarity from public figures, such as Diana, Princess of Wales. When opening the first specialist HIV ward in the UK in 1987, she met and was photographed shaking hands with a patient diagnosed with AIDS. Not only did she show the public there is no harm in touching people with AIDS, she also demonstrated her support to the patients and to the LGBTQIA+ community*.
An aspect that is often forgotten when talking about the HIV epidemic is the involvement of women. In 1986, 7% of HIV patients in the US were female, but research neglected these women by focussing on how the virus presented in men. There was little data on how the infection caused damage to women, both epidemiologically and symptomatically. Additionally, the CDC disease definition did not include symptoms seen in women infected with HIV. For example, thrush in the mouth of infected men caused by an opportunistic fungal infection (Candida Albicans) was included for an AIDS diagnosis, whereas vaginal soreness caused by the same fungus was excluded. Unsurprisingly, women were also refused from research studies, which again contributed to the lack of understanding of how the virus affected them. Women were excluded from an epidemic that did not discriminate in gender, so instead they participated in activism—standing up for themselves and for the LGBTQIA+ community.
Alexis Danzig joined ACT UP after her father died of AIDS. As a lesbian herself, she felt she was part of the battle. ACT UP provided a safe haven for “gay men, lesbians, and their straight allies”, a place where they could express their anger and fear about the discrimination and homophobia they encountered. In a time of governmental ignorance, marginalised communities came together to spread HIV awareness. As part of ACT UP, Danzig and other women concentrated on the inclusion of women by ensuring symptoms that affected feminised reproductive systems were included in the HIV and AIDS disease definitions, advocating for the admittance of women in drug trials, as well as telling the stories of the women affected. In San Diego, women set up the ‘blood sisters’ group. People suffering from AIDS become severely anaemic and may need multiple blood transfusions as a result. The blood sisters organised blood donation drive-throughs to ensure there was a continuous supply of blood for the HIV and AIDS patients.
“The famous “silence=death” poster created in 1986 by ACT UP activists was used to urge the governments to take action; by remaining silent more and more people would die. ”
Women, and specifically women who were themselves part of the LGBTQIA+ community, played a vital role in caring for AIDS patients. In the early stages of the epidemic, patients infected with HIV and who were showing AIDS symptoms were often locked in separate wards, receiving minimal and very distant care. With no cure available, doctors did not know how to treat the deadly infection and some refused to go near patients at all. It was often nurses, almost all women and many of them lesbians, who stepped in to provide effective and compassionate care. Besides caring for the men until they died, they provided company when their families refused to visit, and also helped arrange their funerals. These nurses did so much more than just taking care of the dying men; they ensured that they were loved, and part of a community willing to fight against hate, fear, and stigmas.
Image credit: CDC
“It was often nurses, almost all women and many of them lesbians, who stepped in to provide effective and compassionate care.”
The first treatment for HIV was approved in 1987. However, the drug, azidothymidine (AZT), only extended the lives of patients, it was not a cure. Additionally, HIV is a “clever” virus; it mutates when put under pressure, like when it’s being challenged by drugs. So when AZT was introduced, the virus quickly became resistant, just like it became resistant to the other single-drug treatments that followed. In the mid-1990s a new type of treatment plan was designed, combining multiple single-drug treatments together. This highly active antiretroviral therapy (HAART or ART) stops the virus from multiplying by intervening at different stages of the viral replication cycle. The drugs keep the viral count so low that the virus is no longer able to cause damage in the immune system, preventing the progression from HIV into AIDS. The low viral counts also mean that HIV is no longer transmissible from person to person. Additionally, the simultaneous administration of various therapies hinders the virus from mutating into resistance. ART was shown to be highly effective and to this day still is the golden standard for HIV treatment: patients are able to live healthy lives as long as they stay on the treatment.
This brings us back to Bruno, who is able to live a normal life with HIV. When Bruno was first diagnosed, he thought he “was going to die”. Bruno decided to get tested for the virus when one day he got very sick: “I was in bed with body pains, chills, and was generally feeling awful” he recollects. After having unprotected sex, he had a slight suspicion, even though his partner “swore he did not have the virus”. When Bruno told his partner at the time about his diagnosis, “he said he was going to get a test, and within half an hour he sent me a text back saying he was negative”, which as Bruno notes, “just did not add up”. The secrecy, and perhaps shame, Bruno experienced with his partner goes to show how negatively HIV and AIDS are still perceived today.
Image credit: Wiki Commons
Bruno’s treatment plan was set up quickly after his diagnosis, “I came back for a second test a week after the first one, two weeks later I started my treatment, and after a month the virus was no longer detectable in my blood”. Although physically Bruno was now well, mentally he was struggling: “I had a lot of anxiety and insomnia after the diagnosis, I cried a lot, and I didn’t know anyone who was also HIV positive, so I didn’t have anybody to talk to”. When Bruno decided to talk to a friend about it, “he said to me: “don’t worry, me too"", leaving him confused and wondering why they had never spoken about it before. The isolation that Bruno experienced in the first few weeks after his diagnosis spurred him to post his diagnosis on Facebook: “I didn’t want anyone to go through what I did, it is not some secret club that we can’t talk about”. The response was surprising: “lots of my friends reached out telling me they were HIV positive as well. It’s much more common than you think.” He also received no negative replies, “there was no hostility at all; I knew that the post was not something that was going to haunt me in the future, it will only help people―even now when people come up to me after they have found out about my diagnosis, they only have nice things to say”.
“HIV affects a wide range of individuals, but many still see it to be a virus of the LGBTQIA+ community. With homosexuality still criminalised in certain countries, it prevents people from getting tested in fear of revealing their sexual orientation. ”
We have come a long way since the 1980s, but to understand HIV and AIDS today, we must understand what it meant 40 years ago. Stigmas don’t just disappear, they need to be confronted through educating not only the public, but also the media and governments. Bruno is very lucky that he has not experienced any of the negative stigmas associated with a HIV diagnosis. His openness about his diagnosis has helped him come to terms with being HIV positive, pointing out that “you will feel so alone when you don’t talk about your diagnosis”. By spreading awareness, Bruno is trying to show other patients that they are not only not alone, but that reaching out to others will make living with the virus easier. In Bruno’s opinion, when people decide to hide their diagnosis they can end up making their lives harder, because it confirms negative beliefs that they are unlovable and unaccepted, “which will make them very unhappy”.
However, Bruno recognises that disclosing HIV status might be safer for some individuals than others. Lack of information, education, and conversation can make for an unsafe environment for a person living with HIV, as it can lead to discrimination, violence, and even loss of healthcare. HIV affects a wide range of individuals, but many still see it to be a virus of the LGBTQIA+ community. With homosexuality still criminalised in certain countries, it prevents people from getting tested in fear of revealing their sexual orientation. The isolation of people living with HIV has a negative impact on their mental health and takes a toll on their quality of life. The stigmas surrounding HIV prevent the open conversations that are so desperately needed, especially when it comes to testing. Fear of experiencing discrimination can stop people from getting tested and treated which can continue to drive the epidemic.
The World Health Organization’s (WHO) main HIV message is that when the infection is undetectable, it is not transmissible, thus preventing further spread of the disease. However, what about when testing or treatment is not available? In Sub-Saharan Africa, AIDS is now the leading cause of death. Testing has not been widely available and, again, negative stigmas prevent people from getting tested. If people do get tested, treatment can be scarce because of the high prices and low distribution rates in many African regions. To increase testing and access to treatment, the Joint United Nations Programme on HIV and AIDS (UNAIDS) set the 95-95-95 targets; “worldwide, 95% of people living with HIV know their status, 95% of people who know their status are on ART, and 95% of people on ART show viral suppression”. A huge difference has been made already, but the goals have not yet been reached. By providing education, and implementing testing and treatment programs, the UNAIDS hopes to reach these goals by 2030.
Although there is no cure, it is important to also focus on the positives; being on the treatment has allowed Bruno to start a family, and as he says: “it is giving me the chance to grow old with my husband”. The development of ART has allowed affected people to go from dying from AIDS to living with HIV. Bruno has undoubtedly been lucky in his experience sharing his diagnosis, and is an example of the benefits of starting a conversation if you are able to.
The HIV epidemic is not over. There is no cure, and in terms of acceptance there still is a long way to go. As noted by the WHO, there is a shortcoming when it comes to conversation and education about HIV. Fear and stigmas associated with the disease are still interfering with the progress. Bruno has shown us that by being open to talking about the condition, a difference can be made. The “silence=death” poster made during the first awareness campaigns still has an impactful message. In the 80s, the message was intended to convince the government to increase funding. Nowadays, it is used to assure people living with HIV that open conversations can be a life-changing, and also positive and liberating, experience.
*At the time, these identities were put under the umbrella of ‘gay men’. This article is focussed on gay and lesbian people, however there are also lots of heterosexual people that are living with HIV. In addition to this, other marginalised groups that have not been mentioned in this article are disproportionately affected by the virus, such as people from BAME groups, intravenous drug users, and sex workers.
If you are worried about having contracted HIV/AIDs, see https://www.nhs.uk/conditions/hiv-and-aids/diagnosis/
If you want to learn about disclosing HIV status and advice on how to do so, see https://www.nat.org.uk/sites/default/files/publications/YourVoice.pdf
If you are struggling with your mental health, see https://www.mentalhealth.org.uk/explore-mental-health/get-help
If you are interested in finding out more about what it was like during the first years of the HIV and AIDS emergence, the mini-series ‘It’s a sin’ portrays the lives of three young gay men living in London and their struggles dealing with the virus and its stigmas.