Combatting vaccine hesitancy in 2021: A viral pandemic gone viral
14 May 1796. This was the day the very first vaccine was administered by Dr Edward Jenner. It was the day the eradication of smallpox began. It was the day the modern vaccine immunology era began. It was also the day vaccine oppositions arose.
Image Credit: Wikimedia Commons
Edward Jenner
Dr Edward Jenner is known as the pioneer of vaccine immunology because of his ground-breaking experiments. At the time smallpox was an endemic disease in most regions of the world. However, Jenner noticed that the only people not contracting smallpox were milkmaids. He hypothesized this was because they had been exposed to the far less virulent cowpox and therefore had some immunity to smallpox. Additionally, it was known that people who recovered from smallpox developed immunity as well. To test his hypothesis, Jenner took matter from a cowpox lesion found on the hand of a milkmaid, with which he inoculated an 8-year-old boy. This method later became known as ‘variolation’. Two months later, on the 1st July, he inoculated the boy again, but this time using matter from a smallpox lesion. The boy did not develop disease. Edward Jenner’s hypothesis was confirmed: the boy had established immunity.
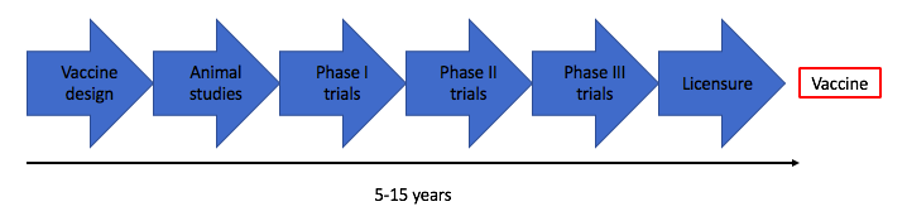
Since Jenner’s discovery, vaccine development has changed exceptionally. The original smallpox vaccine was classified as a natural vaccine. Over the years other vaccine types were created, including live attenuated vaccines (chickenpox vaccine), conjugate vaccines (MenC vaccine), and purified subunit vaccines (hepatitis B vaccine). Although the end products are different, the so-called ‘developmental pipeline’ is the same for every vaccine. It outlines the different phases of vaccine development, starting with the design and animal studies, and ending with large phase III studies and licensure (Image 1). With every step in the pipeline, the research cost increases. Typically, development of a vaccine takes anywhere between 5 to 15 years. Vaccine design is generally the stage that requires the most time, especially when there is no prior knowledge of the infectious disease; laboratory research, for example, often lasts 2 to 4 years.
Image Credit: Tessa de Mooij
Image 1. Typical vaccine development pipeline
The Oxford/AstraZeneca COVID-19 vaccine was designed over a weekend. This was achieved by predicting which infectious disease posed the greatest risk to the public. This list of “pathogens of concern” is managed by the World Health Organisation (WHO) and includes pathogens which have the potential to cause pandemics. Consequently, research can be focussed on vaccine design before an outbreak happens, so when the time comes, vaccine trials can be set up quickly. Part of the vaccine design is development of a delivery method to our immune system. A group of researchers at the Jenner Institute (located in Oxford University) studied the process of vaccine delivery by adenovirus-based vectors. Viral vectors are used to optimally activate our immune system against specific parts (antigens) of an infectious disease to induce a memory response, and thus protect us against future exposure. Nonetheless, it can take a long time to find a vector and antigen combination which induces the best protective response in our bodies. In 2018, the ChAdOx1 vector was developed, which resulted in strong protection when combined with MERS antigens (closely related to COVID-19 antigens). So, when the COVID-19 pandemic was declared, the vaccine delivery platform had already been established. All that was left to do was combining the vector with COVID-19 antigens and test it in trials to create the vaccine we now know as the AstraZeneca vaccine. Although the quick vaccine roll-out was applauded by many, there are some who still refuse to take the vaccine.
Image Credit: Wellcome collection
Image 2. Color etching by James Gillray, 1803
The main reasons for vaccine refusal include people not trusting the research, not trusting the vaccine’s safety, and not trusting their respected government. A lack of trust, and perhaps of education, seem to be the common denominators for vaccine hesitancy. This vaccine distrust is not new. When Jenner first published his variolation results as an approach to protect people from smallpox, opposition quickly emerged. A cartoon was published which pictured vaccinated people with cow-like features, implying that the use of cowpox as a means of protection was risky and unhealthy (Image 2). A similar cartoon was released not long after the first COVID-19 vaccines emerged. This time it showed people turning into monkeys, as the previously mentioned ChAdOx1 vector is based on a chimpanzee adenovirus. It has been suggested that the cartoon was first released by Russian social media to discredit the AstraZeneca vaccine and thus promote their own (Sputnik-V) vaccine, however this has not been confirmed.
New to the current pandemic is the social media landscape, with the “anti-vaxxer” movement using social media platforms to its advantage. Not only do they question the role of the government and the restrictions they have implemented, but also the speed with which the vaccines were developed. With the circulation of misinformation and fake news all over social media platforms, vaccine hesitancy grew, resulting in 6% of UK adults not wanting the vaccine. People were aware that pre-pandemic vaccine development could take years and therefore questioned how COVID-19 vaccines were developed in a few months. However, and unnoticed by the public, the developmental pipeline transformed when the pandemic hit. As mentioned, researchers were better prepared, with numerous vaccines already under development years ahead of the outbreak. Beside this, the pandemic is a global crisis and the world-wide demand for a vaccine was huge. As a result, the research funds were just as huge: independent news organisation Devex reported that more than 21 trillion US dollars was invested in COVID-19 research world-wide. Previously, researchers would have applied for grants and awaited funding for vaccine research, which can slow down the process. Moreover, it was not just one research group investigating potential COVID-19 vaccines, it was hundreds of groups all over the world working day and night. Both the increase in funds and intensive research sped up vaccine development. The vaccine pipeline might experience similar transformations during future infectious disease outbreaks, if their spread is predicted by the WHO. However, this might not be the case for ‘disease X’—an unknown pathogen that could cause disease in humans with currently unpredictable consequences.
Image Credit: Unsplash
As Heidi Larson—medical anthropologist and professor at the London School of Hygiene and Tropical Medicine—pointed out: it is not lack of preventative techniques that could make the next outbreak even more dangerous, it is the spread of misinformed and manipulated information across social media. How can we prevent this? Or the better question might be: how can we educate people to prevent the spread of misinformation and fake news and avoid vaccine hesitancy? It is important to start from the source. Fake news circulates and influences people through social media. Over the past year, numerous social media platforms such as Facebook, Instagram, and Twitter have been actively removing posts involving false information. However, removing misinformation is not enough—it needs to be replaced with accurate information. In an attempt to do so, the WHO set up an active COVID-19 campaign on their social media and website. They also asked the help of celebrities/influencers and their online platforms to help educate the people and urge them to get the vaccine, like Elton John did for the National Health Service (NHS) advertisement. In addition, numerous health care professionals have used their platforms to help inform the public about COVID-19 and the vaccines. An example is the Dutch physician Diederik Gommers. At the beginning of the pandemic his role mainly involved being part of the Outbreak Management Team (OMT) and advising the Dutch government. A year later, he is known for his honest and understandable explanations to the public involving pandemic issues. Similarly, the UN set up Team HALO, an online platform of scientists and health care professionals from all over the world. The professionals devote their time to answering questions about COVID-19 and the current vaccines, and the team produces videos with explanations and facts on the safety of vaccines. So, vaccine hesitancy can be interfered with through the spread of accurate information and research transparency.
Although the previously mentioned points apply to the majority of people, it might not apply to everyone. What about those that do not have access or have limited access to the internet? What about global ethnic majority groups that have been wronged by their government before? Such as those in the Tuskegee study, where nearly 400 Black men thought they were being treated for syphilis, when actually their disease progression was being observed. These are the questions that need to be considered and that need to be thought about before the next outbreak.
Overall, to prevent vaccine hesitancy, educating the public is key. It is healthy for people to question research, but it is even better that those questions are answered by professionals in a comprehensive manner. From this pandemic we have learned what is required in a vaccine hesitancy prevention strategy, and that a successful one must consider everyone’s needs and views.